Introduction
Does gender matter when calculating BMI? Since BMI for Men vs Women often have different body compositions, muscle mass distributions, and fat storage patterns, it’s a fair question that many people ask when trying to understand their health status. The relationship between biological sex and BMI interpretation has become increasingly important as we better understand how gender differences affect health outcomes.
This comprehensive article explains the relationship between BMI, gender, and health risks, exploring how biological differences between men and women might influence BMI accuracy and interpretation. We’ll examine the science behind gender-specific body composition, discuss when these differences matter most, and provide practical guidance for both men and women using BMI as a health assessment tool.
Table of Contents
Understanding Gender and BMI: The Scientific Foundation
The Body Mass Index was originally developed using data from predominantly male populations in the 19th century, yet it’s applied universally today. This historical context raises important questions about whether a one-size-fits-all approach truly serves both men and women equally well.
Research over the past several decades has revealed significant differences in how men and women store fat, build muscle, and respond to dietary and exercise interventions. These differences stem from various factors including hormones, genetics, evolutionary biology, and lifestyle patterns that can significantly impact how BMI should be interpreted.
Are BMI Categories the Same for Men & Women?
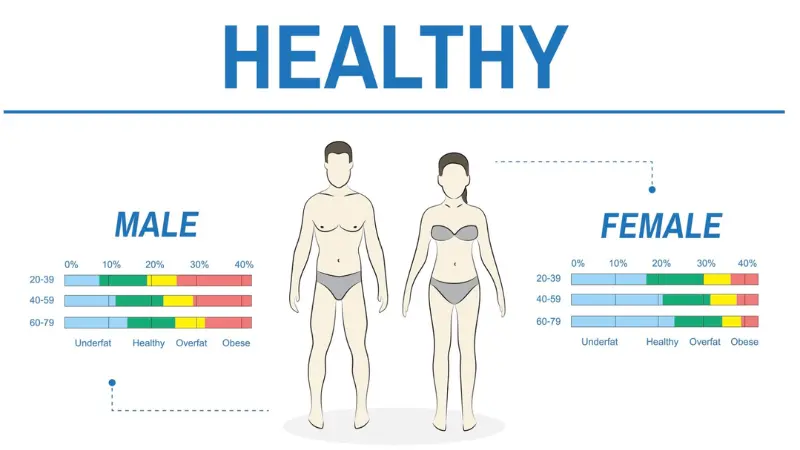
Yes, the standard BMI categories apply equally to men and women across all major health organizations worldwide. The World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), and other international health bodies use identical BMI ranges for both genders.
| Category | BMI Range | Health Risk Level |
|---|---|---|
| Underweight | < 18.5 | Increased risk of malnutrition, osteoporosis |
| Normal weight | 18.5 – 24.9 | Lowest risk of chronic diseases |
| Overweight | 25 – 29.9 | Increased risk of cardiovascular disease |
| Obese | 30+ | Significantly increased risk of multiple conditions |
Why are the categories the same?
- Standardization: Universal categories allow for consistent health assessments across populations
- Research basis: Large-scale studies have shown similar relationships between BMI and health outcomes in both men and women
- Practical application: Healthcare providers and researchers need consistent metrics for diagnosis and treatment
- Population health: Public health initiatives require standardized measurements for effective implementation
However, this standardization doesn’t mean that BMI affects men and women identically. The interpretation and accuracy of BMI can vary significantly between genders due to fundamental biological differences.
Comprehensive Body Composition Differences
Men’s Body Composition Characteristics
Muscle Mass Distribution:
- More overall muscle mass – Men typically have 30-40% more muscle mass than women
- Upper body strength – Significantly higher muscle concentration in arms, shoulders, and chest
- Testosterone influence – Higher testosterone levels promote muscle development and maintenance
- Bone density – Generally higher bone density contributing to overall body weight
Fat Distribution Patterns:
- Android fat distribution – Fat tends to accumulate around the abdomen (apple-shaped)
- Visceral fat – Higher tendency to store fat around internal organs
- Lower body fat percentage – Men typically have 10-15% body fat at healthy weights
- Metabolic implications – Abdominal fat distribution increases cardiovascular risk
Physiological Factors:
- Higher basal metabolic rate – More muscle mass means higher calorie burn at rest
- Growth hormone levels – Higher levels support muscle maintenance
- Insulin sensitivity – Generally better insulin sensitivity, especially when lean
Women’s Body Composition Characteristics
Fat Distribution Patterns:
- More body fat overall – Women typically have 20-25% body fat at healthy weights
- Gynoid fat distribution – Fat tends to accumulate in hips, thighs, and buttocks (pear-shaped)
- Subcutaneous fat – Higher proportion of fat stored under the skin rather than around organs
- Essential fat – Women require higher body fat percentages for reproductive health
Muscle Mass Characteristics:
- Less overall muscle mass – Women typically have 60-70% of men’s muscle mass
- Lower body strength – Relatively stronger legs compared to upper body
- Estrogen influence – Estrogen affects fat storage and muscle development patterns
- Bone density variations – Generally lower bone density, especially post-menopause
Hormonal Influences:
- Estrogen effects – Promotes fat storage in hips and thighs
- Progesterone impact – Affects water retention and body composition
- Menstrual cycle variations – Monthly hormonal fluctuations affect weight and body composition
- Menopause transitions – Hormonal changes can shift fat distribution patterns
How Gender Differences Affect BMI Accuracy
Potential BMI Misinterpretations in Men
Athletic and Muscular Men: Since BMI doesn’t measure fat or muscle directly, men with high muscle mass may appear overweight or obese on BMI scales despite having very low body fat percentages. This is particularly common in:
- Strength athletes – Powerlifters, bodybuilders, and football players
- Military personnel – Often have high muscle mass from training requirements
- Construction workers – Physical labor builds significant muscle mass
- Fitness enthusiasts – Regular weightlifting can increase muscle mass substantially
Real-world examples:
- Professional rugby players often have BMIs over 30 despite body fat percentages under 12%
- Military personnel may be classified as overweight despite being in peak physical condition
- Men who strength train regularly may see their BMI increase as they build muscle
Health implications:
- High muscle mass actually protects against metabolic diseases
- Muscular men may have better insulin sensitivity than their BMI suggests
- Cardiovascular fitness may be excellent despite “overweight” BMI classification
Potential BMI Misinterpretations in Women
Normal-Weight Obesity in Women: Women with low muscle mass but high fat percentage may appear normal on BMI scales while still facing health risks. This condition, known as “normal-weight obesity,” is more common in women and includes:
- Sedentary women – Lack of exercise leads to muscle loss and fat gain
- Older women – Age-related muscle loss (sarcopenia) combined with fat gain
- Women with hormonal imbalances – Conditions affecting metabolism and body composition
- Those with restrictive dieting history – Repeated dieting can reduce muscle mass
Specific concerns:
- Women may have healthy BMIs but unhealthy body fat percentages (over 32%)
- Metabolic health markers may be poor despite normal BMI
- Risk of diabetes and cardiovascular disease may be higher than BMI suggests
Hormonal influences on BMI accuracy:
- Pregnancy and postpartum – Significant body composition changes
- Menopause – Hormonal changes affect fat distribution and muscle mass
- PCOS – Polycystic ovary syndrome affects weight and body composition
- Thyroid disorders – More common in women and affect metabolism
Age-Related Gender Differences in BMI
Young Adults (18-30 years)
Men:
- Peak muscle mass development
- Most accurate BMI readings for health assessment
- Athletic performance often at its highest
- Testosterone levels support muscle maintenance
Women:
- Reproductive years may affect body composition
- Pregnancy and childbirth can impact BMI accuracy
- Menstrual cycle variations affect weight measurements
- Generally good BMI accuracy for health assessment
Middle Age (30-50 years)
Men:
- Gradual muscle loss begins (1-2% per year after 30)
- Testosterone levels start declining
- Increased risk of abdominal fat accumulation
- BMI accuracy may decrease for very active individuals
Women:
- Perimenopause and menopause significantly impact body composition
- Hormonal changes shift fat distribution from hips to abdomen
- Muscle loss accelerates without intervention
- BMI may underestimate health risks during hormonal transitions
Older Adults (50+ years)
Men:
- Significant muscle mass loss if not maintained through exercise
- Increased risk of normal-weight obesity
- BMI may overestimate health risks in very fit older men
- Bone density changes affect total body weight
Women:
- Post-menopausal hormonal changes dramatically affect body composition
- Higher risk of osteoporosis affecting BMI calculations
- Increased abdominal fat storage changes health risk profiles
- BMI may underestimate health risks due to muscle loss
Should You Interpret BMI Differently by Gender?
Current Medical Consensus
Not necessarily — but consider body composition, especially if you’re an athlete or older adult. The medical community generally maintains that BMI categories should remain consistent between genders for several reasons:
Supporting arguments:
- Large-scale studies show similar relationships between BMI and health outcomes in both men and women
- Standardization benefits outweigh potential gender-specific accuracy improvements
- Practical application requires consistent metrics across populations
- Healthcare efficiency benefits from universal screening tools
However, context matters:
- Individual assessment should always consider gender-specific factors
- Additional measurements become more important when gender differences are significant
- Professional evaluation can account for body composition differences
- Lifestyle factors should be considered alongside BMI results
When Gender Differences Matter Most
High-priority situations for gender-specific interpretation:
- Athletic populations – Both male and female athletes may have misleading BMIs
- Older adults – Age-related changes affect men and women differently
- Clinical assessments – Healthcare providers should consider gender-specific factors
- Specialized populations – Military, fitness professionals, and others with unique body compositions
Moderate-priority situations:
- General health screening – BMI provides reasonable estimates for most people
- Weight management – Both men and women can use BMI for goal setting
- Population health studies – Gender differences often average out in large groups
Learn more in our Is BMI Accurate? article for detailed information about BMI limitations and alternatives.

Practical Tips for Both Genders
Universal Recommendations
✅ Use BMI as a guideline – Consider it one tool among many for health assessment ✅ Combine it with waist measurements – Waist circumference provides additional insights into health risks ✅ Focus on overall health, not just the number – Consider fitness level, energy, and overall well-being ✅ Track trends over time – Changes in BMI can be more meaningful than single measurements ✅ Consult healthcare providers – Professional interpretation considers individual factors
Gender-Specific Recommendations
For Men:
- Consider muscle mass – If you’re very active or muscular, BMI may overestimate health risks
- Monitor waist circumference – Men are more prone to abdominal fat accumulation
- Focus on strength maintenance – Preserve muscle mass through resistance training
- Watch for middle-age spread – Hormonal changes can affect body composition after 40
For Women:
- Consider hormonal factors – Menstrual cycle, pregnancy, and menopause all affect body composition
- Monitor throughout life stages – Different life phases may require different health assessments
- Focus on muscle preservation – Women are more prone to age-related muscle loss
- Consider bone health – Osteoporosis risk affects both weight and overall health
Advanced Assessment Strategies
Complementary Measurements:
- Waist-to-hip ratio – Particularly important for women due to different fat distribution patterns
- Body fat percentage – More accurate than BMI for both genders, especially athletes
- Muscle mass assessment – Especially important for men with high muscle mass
- Metabolic markers – Blood pressure, cholesterol, and blood sugar provide additional context
Professional Assessments:
- DEXA scans – Provide detailed body composition analysis
- Bioelectrical impedance – Estimates body fat percentage
- Hydrostatic weighing – Accurate body composition measurement
- Medical evaluation – Comprehensive health assessment beyond BMI
Emerging Research and Future Directions
Gender-Specific BMI Research
Current studies investigating:
- Ethnic variations – How gender differences vary across different populations
- Hormonal influences – Detailed understanding of how hormones affect BMI accuracy
- Age-specific considerations – How gender differences change throughout the lifespan
- Genetic factors – How genetics influence gender-specific body composition
Potential future developments:
- Personalized BMI categories – Gender and age-specific BMI ranges
- Hormonal adjustments – BMI calculations that account for hormonal status
- Genetic BMI – Personalized BMI based on genetic predispositions
- Technology integration – Wearable devices that provide real-time body composition data
Implications for Healthcare
Current trends:
- Individualized medicine – Moving toward personalized health assessments
- Multi-metric approaches – Using multiple measurements rather than BMI alone
- Gender-specific research – Increasing focus on how medical conditions affect men and women differently
- Precision health – Tailoring health recommendations to individual characteristics
Conclusion
BMI works the same for everyone in terms of calculation and categories — but understanding your unique body composition helps you interpret it better. While the standard BMI categories apply equally to men and women, the underlying biological differences between genders can significantly affect how accurately BMI reflects your health status.
Men with high muscle mass may find that BMI overestimates their health risks, while women with low muscle mass but higher body fat percentages may find that BMI underestimates their risks. These differences become particularly important for athletes, older adults, and those with unique body compositions.
The key is to use BMI as a starting point for health assessment, not the final word. Combine BMI with other measurements like waist circumference, consider your individual circumstances including age, activity level, and health history, and work with healthcare providers who can provide personalized interpretations.
Remember that health is multifaceted and cannot be captured by any single measurement. Focus on overall wellness, including physical fitness, mental health, and lifestyle factors, rather than becoming fixated on any single number.
Check your BMI now with our BMI Calculator NHS, but remember to interpret the results in the context of your individual gender-specific factors and overall health picture.