Introduction
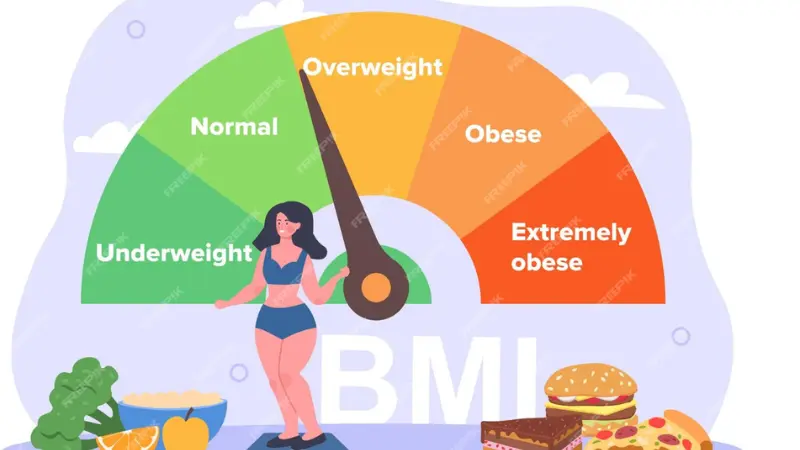
BMI is simple to calculate, but does it really measure your health? Many experts debate whether BMI is accurate for everyone, and this question has become increasingly important as we better understand the complexities of human body composition and health assessment.
In this comprehensive guide, we explore Is BMI Accurate?, its pros and cons, and alternatives you can consider for a more complete picture of your health. We’ll examine real-world scenarios where BMI works well and where it falls short, helping you make informed decisions about using this popular health metric.
Table of Contents
Understanding BMI’s Role in Health Assessment
Body Mass Index (BMI) was developed in the 1830s by Belgian mathematician Adolphe Quetelet, originally called the “Quetelet Index.” It gained popularity in the 1970s when researchers needed a simple way to categorize weight status across large populations. Today, BMI remains one of the most widely used health screening tools globally, but its accuracy and applicability continue to be subjects of scientific debate.
The BMI formula divides your weight in kilograms by your height in meters squared (kg/m²). This mathematical relationship provides a standardized way to compare weight status across different individuals, regardless of their absolute weight or height.
Why BMI is Popular
BMI’s widespread adoption stems from several practical advantages that make it accessible to healthcare providers, researchers, and individuals worldwide:
Simplicity and Accessibility:
- Quick & easy to calculate – Requires only basic math or online calculators
- Requires only height & weight – No expensive equipment or specialized training needed
- Universally applicable – Can be used anywhere in the world with consistent results
- Cost-effective – No additional testing or laboratory work required
Clinical and Research Applications:
- Helps categorize health risks – Provides standardized categories for medical assessment
- Population health studies – Enables large-scale epidemiological research
- Insurance and medical screening – Used by insurance companies and healthcare systems
- Public health initiatives – Helps track obesity trends and health outcomes
Historical data availability – Decades of research have established BMI’s relationship with various health outcomes, making it a valuable tool for comparing historical trends and predicting future health risks.
Comprehensive Pros of BMI
Advantages for Healthcare Providers
✅ Easy to use – Healthcare providers can quickly assess patients without specialized equipment or extensive training. This efficiency is particularly valuable in busy clinical settings or resource-limited environments.
✅ Standardized categories – The universal BMI categories (underweight, normal, overweight, obese) provide consistent language for discussing weight status across different healthcare systems, countries, and medical specialties.
✅ Predicts risk of diseases in large populations – Extensive research has established strong correlations between BMI and various health conditions, including:
- Type 2 diabetes
- Cardiovascular disease
- Certain cancers
- Sleep apnea
- Osteoarthritis
- Gallbladder disease
Population-Level Benefits
✅ Epidemiological research – BMI enables researchers to study health trends across large populations, track obesity epidemics, and identify risk factors for chronic diseases.
✅ Public health policy – Governments and health organizations use BMI data to develop public health initiatives, allocate resources, and create targeted interventions.
✅ Insurance and screening – BMI provides a standardized metric for insurance companies to assess risk and for employers to implement workplace wellness programs.
Individual Benefits
✅ Self-monitoring tool – Individuals can easily track their BMI over time to monitor weight changes and health progress.
✅ Motivation and goal-setting – BMI categories provide clear targets for weight management goals and lifestyle changes.
✅ Initial health assessment – BMI serves as a starting point for individuals to assess their weight status and consider whether lifestyle changes might be beneficial.
Detailed Cons of BMI
Body Composition Limitations
❌ Doesn’t distinguish between fat and muscle – This is perhaps BMI’s most significant limitation. Muscle tissue is denser than fat tissue, meaning two people with identical BMIs can have vastly different body compositions. A bodybuilder with 8% body fat might have the same BMI as someone with 25% body fat.
❌ Doesn’t account for body composition – BMI cannot differentiate between:
- Subcutaneous fat (under the skin) vs. visceral fat (around organs)
- Lean muscle mass vs. fat mass
- Bone density variations
- Water retention and hydration status
❌ Ignores fat distribution – Research shows that abdominal fat (apple-shaped body) poses greater health risks than hip and thigh fat (pear-shaped body), but BMI doesn’t account for these differences.
Demographic Limitations
❌ May misclassify athletes or older adults – Athletes often have high muscle mass that elevates their BMI despite having low body fat. Conversely, older adults may have normal BMIs despite having high body fat percentages due to age-related muscle loss.
❌ Gender differences – Men typically have more muscle mass and less body fat than women at the same BMI, but the standard categories don’t account for these differences.
❌ Ethnic variations – Different ethnic groups have varying body compositions and health risks at the same BMI levels:
- Asian populations may have higher health risks at lower BMIs
- African Americans may have different muscle-to-fat ratios
- Some Pacific Islander populations naturally have higher BMIs without corresponding health risks
Clinical Limitations
❌ Static measurement – BMI provides a snapshot in time but doesn’t reflect changes in body composition that occur with aging, exercise, or medical conditions.
❌ Doesn’t measure metabolic health – Someone can have a normal BMI but still have metabolic syndrome, insulin resistance, or other health issues.
❌ Psychological impact – Overemphasis on BMI can lead to unhealthy behaviors, eating disorders, or negative self-image, particularly in young people.
Who Might BMI Mislead?
Athletes and Active Individuals
Athletes: High muscle mass may appear as overweight or obese on BMI scales. Professional athletes in sports requiring significant muscle mass (football players, weightlifters, rugby players) often have BMIs in the overweight or obese range despite having very low body fat percentages.
Fitness enthusiasts: Regular strength training can increase muscle mass to the point where BMI becomes misleading. Someone who has successfully replaced fat with muscle through exercise might see their BMI increase despite improving their health.
Specific examples:
- Professional football players often have BMIs over 30 despite body fat percentages under 10%
- Bodybuilders may have BMIs over 35 while being in peak physical condition
- Swimmers and gymnasts may have misleading BMI readings due to their unique body compositions
Elderly Population
Elderly individuals: Low muscle but high fat may appear “healthy” on BMI scales. Age-related muscle loss (sarcopenia) can result in normal BMIs despite having high body fat percentages and increased health risks.
Specific concerns:
- Muscle mass naturally decreases with age (3-8% per decade after age 30)
- Bone density changes affect overall weight
- Metabolism slows, potentially changing body composition
- Medications may affect weight and body composition
Different Ethnicities and Populations
Asian populations: Research shows that Asian individuals may have higher health risks at lower BMIs compared to other ethnic groups. The WHO has suggested modified BMI categories for Asian populations:
- Overweight: BMI ≥ 23
- Obese: BMI ≥ 27.5
African Americans: Studies indicate that African Americans may have different muscle-to-fat ratios and bone density compared to other populations, potentially affecting BMI accuracy.
Hispanic populations: Some research suggests that Hispanic individuals may have different body fat distributions that aren’t captured by BMI alone.
Pacific Islanders: Some Pacific Islander populations naturally have higher BMIs without corresponding increases in health risks, possibly due to genetic factors and body composition differences.
Comprehensive Alternatives to BMI
If you want a more accurate picture of your health status, consider these alternatives and complementary measures:
Waist-to-Hip Ratio (WHR)
How it works: Divide your waist circumference by your hip circumference. This ratio indicates fat distribution and can predict health risks better than BMI alone.
Advantages:
- Identifies abdominal obesity, which is more strongly linked to health risks
- Simple to measure at home
- Accounts for body shape differences
Healthy ranges:
- Women: WHR < 0.85
- Men: WHR < 0.90
Body Fat Percentage
How it works: Measures the proportion of your body weight that consists of fat tissue. This can be measured through various methods including bioelectrical impedance, skinfold calipers, or more advanced techniques.
Advantages:
- Directly measures what BMI attempts to estimate
- Accounts for muscle mass differences
- More accurate for athletes and active individuals
Healthy ranges:
- Women: 16-24% (athletes), 20-28% (general population)
- Men: 6-17% (athletes), 10-22% (general population)
Waist Circumference
How it works: Measures the circumference of your waist at the narrowest point. This simple measurement can predict health risks independent of BMI.
Advantages:
- Strong predictor of cardiovascular disease
- Easy to measure consistently
- Accounts for abdominal fat distribution
Risk thresholds:
- Women: > 35 inches (88 cm)
- Men: > 40 inches (102 cm)
Advanced Measurement Techniques
DEXA Scans (Dual-Energy X-ray Absorptiometry):
- Provides detailed body composition analysis
- Measures bone density, muscle mass, and fat distribution
- Considered the gold standard for body composition assessment
- More expensive but highly accurate
Hydrostatic Weighing:
- Measures body density to calculate body fat percentage
- Highly accurate but requires specialized equipment
- Often used in research settings
Air Displacement Plethysmography (Bod Pod):
- Uses air displacement to measure body composition
- Accurate and relatively quick
- Available in some fitness centers and research facilities
Bioelectrical Impedance Analysis (BIA):
- Sends electrical signals through the body to estimate body composition
- Available in home scales and professional devices
- Accuracy can vary based on hydration status
Learn more in our Body Fat vs BMI article for detailed comparisons and guidance on choosing the best measurement method for your needs.
When BMI is Most and Least Accurate
BMI Works Best For:
- Population-level health assessments
- General screening in healthy adults
- Tracking weight changes over time
- Identifying individuals who may benefit from further health evaluation
- Initial health risk assessment
BMI is Less Accurate For:
- Athletes and very active individuals
- Elderly populations
- People with significant muscle mass
- Certain ethnic groups
- Individuals with medical conditions affecting body composition
- Children and adolescents (require age-specific calculations)
Practical Recommendations
For Healthcare Providers:
- Use BMI as a starting point, not the final assessment
- Consider waist circumference alongside BMI
- Account for patient demographics and activity levels
- Look at overall health markers, not just weight status
For Individuals:
- Use BMI as one tool among many
- Consider your personal health history and goals
- Focus on overall health behaviors, not just weight
- Consult healthcare providers for comprehensive assessments
For Specific Populations:
- Athletes: Consider body fat percentage and performance metrics
- Elderly: Focus on maintaining muscle mass and functional ability
- Different ethnicities: Be aware of population-specific risk factors
The Future of Health Assessment
Emerging technologies and research are developing new approaches to health assessment that may complement or replace BMI:
Artificial Intelligence and Machine Learning:
- Advanced algorithms that consider multiple health factors
- Personalized risk assessment based on individual characteristics
- Integration of genetic, lifestyle, and environmental factors
Wearable Technology:
- Continuous monitoring of health metrics
- Real-time body composition tracking
- Integration with other health data for comprehensive assessment
Genetic Testing:
- Understanding individual predispositions to weight gain
- Personalized nutrition and exercise recommendations
- Identification of genetic factors affecting metabolism
Conclusion
BMI is a useful screening tool — but not the whole story. While it provides valuable information for population health studies and initial health assessments, it has significant limitations when applied to individuals, particularly athletes, elderly people, and certain ethnic groups.
The key is to use BMI alongside other measures for a better understanding of your health. Consider your waist circumference, body fat percentage, fitness level, and overall health markers when evaluating your health status. Remember that health is multifaceted and cannot be captured by any single number or measurement.
For the most accurate assessment of your health, work with healthcare providers who can consider your individual circumstances, medical history, and health goals. They can help you interpret BMI results in the context of your overall health and recommend appropriate next steps.
Try our BMI Calculator NHS today to get started, but remember to use the results as just one piece of your health puzzle!